We report a case series of 9 patients with stage III hypertension documented within minutes of vaccination during the first 30 days, of which 8 were symptomatic. … Eight of 9 patients had a history of arterial hypertension with most patients on antihypertensive therapy.
⋮
Due to the patient high throughput in our vaccination center, we do not have prevaccination BP values. However, 8 of 9 patients reported otherwise well controlled hypertension. Our case series suggests that a fraction of hypertensive patients may react with symptomatically significant increases in both systolic and diastolic blood pressure. A stress response is likely in view of the public debate, in addition to pain response and white coat effect—the latter being associated with age and female sex. … An interaction between the S-protein and angiotensin converting enzyme 2 also seems highly unlikely as patients reacted within minutes of the injection, not leaving time for mRNA cellular uptake, translation, and S-protein presentation at the membrane of macrophages and dendritic cells.
But other researchers thought otherwise:
Free-floating Spike proteins [from the COVID-19 vaccines] may interact with angiotensin-converting enzyme 2 (ACE2) receptors leading to internalization, degradation, and dysregulation of the catalytic activities of these receptors. The consequent loss of ACE2 receptor activity leads to a rapid drop in the generation of angiotensin1,7 resulting from inactivation of angiotensin II. The imbalance between angiotensin II (overactivity) and of angiotensin1,7 (deficiency) might play a role in the genesis of acute elevation in blood pressure.
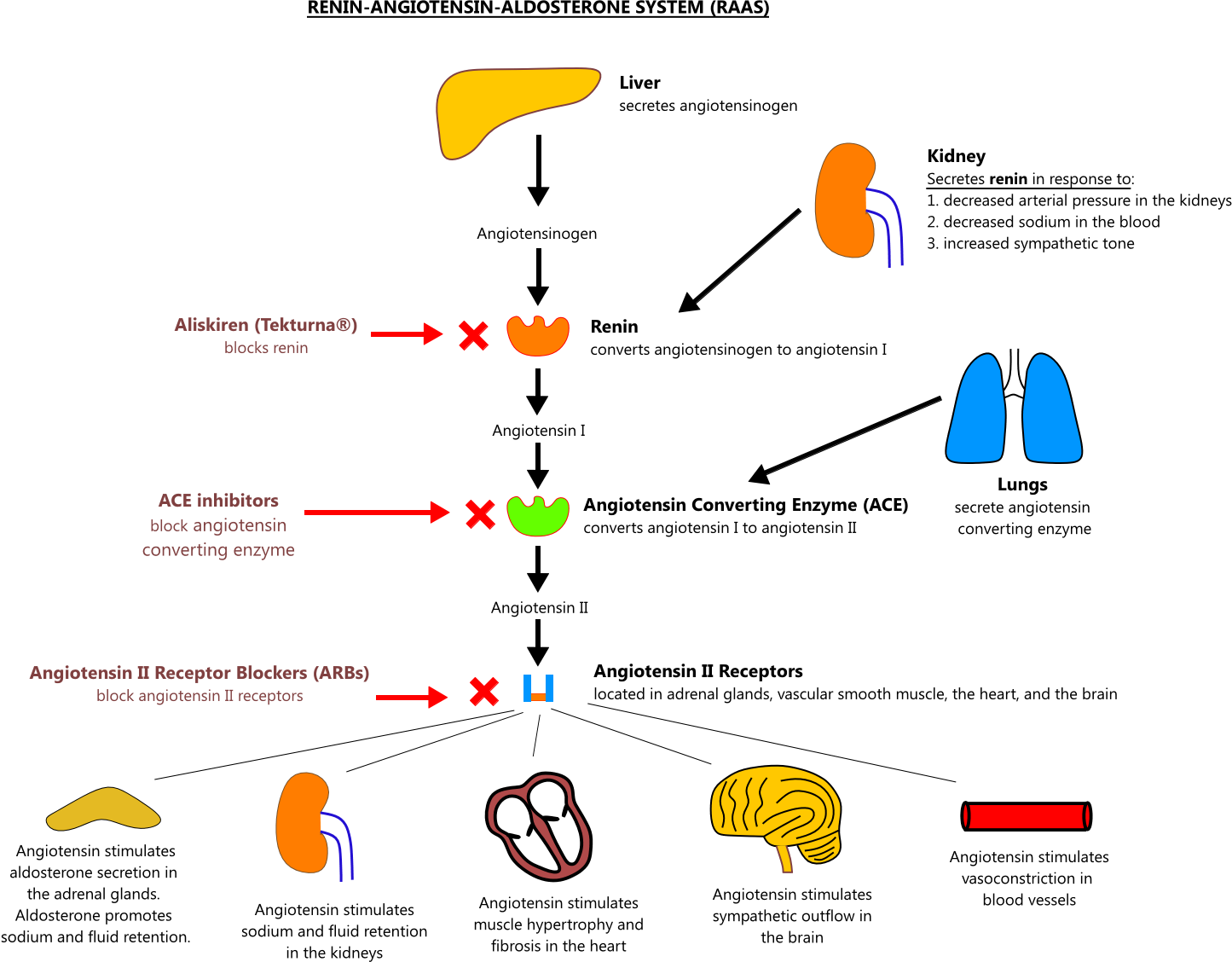
VACCINES AND RENIN-ANGIOTENSIN-ALDOSTERONE SYSTEM
The vigorous immune response stimulated by vaccination produces the activation of the killer cells of our body. This will result in the destruction of the target cell and the release of spike proteins (and their fragments) accumulated in the cytoplasm (“free-floating”).
Since the spike proteins produced by the vaccine appear to be identical to those of SARS-CoV-2 in both morphological and functional terms, it is plausible that they may interact with the ACE2 receptors used by the virus to invade human cells.
The interaction between free-floating spike proteins and ACE2 receptors can therefore trigger the down-regulation mechanism and paralysis of the catalytic functions of the receptors, including the degradation of angiotensin II to angiotensin1,7.
This phenomenon has been well demonstrated in experimental models at platelet level, where SARS-CoV-2 induces a significant reduction of ACE2 receptors, resulting in ATP release and increased aggregation (responsible for thromboembolic events commonly described in COVID-19).
The loss of the catalytic activities of ACE2 receptors at the cell membrane level, mediated by the interaction between Spike proteins and receptors, will produce an increase in angiotensin II values due to reduced transformation into angiotensin1,7 and a dysregulation of the renin-angiotensin-aldosterone system. In addition, the imbalance caused by an overactivity of angiotensin II and the reduction of angiotensin1,7 levels can favor phenomena characterized by an overactivation of the coagulation cascade, inflammation and other adverse reactions including increase in circulating volume and vasoconstriction with an increase in blood pressure values (Figure 1).
Mechanism of DNA and mRNA vaccines and interactions of “free-floating” Spike proteins with ACE2 receptors. A1,7, angiotensin1,7; ACE2, angiotensin converting enzyme 2; AII, angiotensin II; DNA, deoxybonuleic acid; mRNA, messenger ribonucleic acid.
CLINICAL EVIDENCE
The first report that highlighted a link (at least temporal) between vaccination and increase in blood pressure values is that of Meylan et al. These authors described a series of 9 patients (including 7 women and of which 8 with a history of hypertension well controlled by the therapy in place) with the appearance of elevated blood pressure values (compatible with stage III; systolic blood pressure from 168 to 220 mmHg, diastolic blood pressure from 88 to 115 mmHg) after vaccination with Comirnaty (n = 8) and Spikevax (n = 1).
Angiotensin converting enzyme-2 (ACE2) receptors mediate the entry into the cell of three strains of coronavirus: SARS-CoV, NL63 and SARS-CoV-2. ACE2 receptors are ubiquitous and widely expressed in the heart, vessels, gut, lung (particularly in type 2 pneumocytes and macrophages), kidney, testis and brain. ACE2 is mostly bound to cell membranes and only scarcely present in the circulation in a soluble form. An important salutary function of membrane-bound and soluble ACE2 is the degradation of angiotensin II to angiotensin1-7. Consequently, ACE2 receptors limit several detrimental effects resulting from binding of angiotensin II to AT1 receptors, which include vasoconstriction, enhanced inflammation and thrombosis. The increased generation of angiotensin1-7 also triggers counter-regulatory protective effects through binding to G-protein coupled Mas receptors. Unfortunately, the entry of SARS-CoV2 into the cells through membrane fusion markedly down-regulates ACE2 receptors, with loss of the catalytic effect of these receptors at the external site of the membrane. Increased pulmonary inflammation and coagulation have been reported as unwanted effects of enhanced and unopposed angiotensin II effects via the ACE→Angiotensin II→AT1 receptor axis. Clinical reports of patients infected with SARS-CoV-2 show that several features associated with infection and severity of the disease (i.e., older age, hypertension, diabetes, cardiovascular disease) share a variable degree of ACE2 deficiency. We suggest that ACE2 down-regulation induced by viral invasion may be especially detrimental in people with baseline ACE2 deficiency associated with the above conditions. The additional ACE2 deficiency after viral invasion might amplify the dysregulation between the ‘adverse’ ACE→Angiotensin II→AT1 receptor axis and the ‘protective’ ACE2→Angiotensin1-7→Mas receptor axis. In the lungs, such dysregulation would favor the progression of inflammatory and thrombotic processes triggered by local angiotensin II hyperactivity unopposed by angiotensin1-7.
If the spike protein is the culprit, then might we possibly also see this type of high blood pressure reaction in unvaccinated people who are in close relationship with vaccinated people?
Sources:
- April 20, 2020. Paolo Verdecchia, Claudio Cavallini, Antonio Spanevello, and Fabio Angeli. “The Pivotal Link between ACE2 Deficiency and SARS-CoV-2 Infection.” European Journal of Internal Medicine 76 (April): 14–20.

https://doi.org/10.1016/j.ejim.2020.04.037.
Research Journal. - March 25, 2021. Sylvain Meylan, Françoise Livio, Maryline Foerster, Patrick James Genoud, François Marguet, Gregoire Wuerzner, and on behalf of the CHUV COVID Vaccination Center. “Stage III Hypertension in Patients After MRNA-Based SARS-CoV-2 Vaccination.” Hypertension 77 (6): e56–57.

https://doi.org/10.1161/HYPERTENSIONAHA.121.17316.
Research Journal. - June 15, 2021. Martina Zappa, Paolo Verdecchia, Antonio Spanevello, Dina Visca, and Fabio Angeli. “Blood Pressure Increase after Pfizer/BioNTech SARS-CoV-2 Vaccine.” European Journal of Internal Medicine 90 (August 2021): 111–13.

https://doi.org/10.1016/j.ejim.2021.06.013.
Research Journal. - January 2022. Fabio Angeli, Gianpaolo Reboldi, Monica Trapasso, and Paolo Verdecchia. “Ipertensione dopo vaccinazione anti-COVID-19.” [Hypertension after anti-COVID-19 vaccination]. Giornale Italiano di Cardiologia 23 (1): 10–14.

https://doi.org/10.1714/3715.37055,
https://pubmed.ncbi.nlm.nih.gov/34985455/.
Research Journal. - December 12, 2022. Fabio Angeli, Martina Zappa, Gianpaolo Reboldi, Giorgio Gentile, Monica Trapasso, Antonio Spanevello, and Paolo Verdecchia. “The Spike Effect of Acute Respiratory Syndrome Coronavirus 2 and Coronavirus Disease 2019 Vaccines on Blood Pressure.” European Journal of Internal Medicine 109 (March 2023): 12–21.

https://doi.org/10.1016/j.ejim.2022.12.004.
Research Journal.
History of COVID-19 and High Blood Pressure
We learned early on that the vast majority of COVID-19 fatalities had other conditions as well. Top among these is hypertension or high blood pressure.
The new study could provide insight into why Italy’s death rate, at about 8% of total infected people, is higher than in other countries.
The Rome-based institute has examined medical records of about 18% of the country’s coronavirus fatalities, finding that just three victims, or 0.8% of the total, had no previous pathology. Almost half of the victims suffered from at least three prior illnesses and about a fourth had either one or two previous conditions.
More than 75% had high blood pressure, about 35% had diabetes and a third suffered from heart disease.
In this adjusted analysis, use of ACEi/ARB was not associated with testing positive for COVID-19 (OR 0.97, 95% CI 0.81-1.15), but was associated with higher risk of hospital and ICU admission among those testing positive.
— NephJC
Soon, scientists were figuring out that SARS-CoV-2 had a mechanism for causing hypertension.
The virus SARS-CoV-2 employs the Angiotensin-converting enzyme 2 (ACE2), a component of the RAAS (Renin-Angiotensin-Aldosterone System) system, as a receptor for entry into the cells.
Sources:
- March 14, 2020, accessed December 6, 2022. Matthew Sparks, Swapnil Hiremath, Andrew South, Paul Welling, Matt Luther, Jordy Cohen, Brian Byrd, Louise M. Burrell, Daniel Batlle, Laurie Tomlinson, Vivek Bhalla, María José Soler, Sundar Swaminathan, April Pettit, Javid Moslehi, Adam Bress, and Ricky Turgeon. “ACE2 and HYPERTENSION (Should ACE-inhibitors and ARBs be stopped with COVID-19?).” NephJC.

http://www.nephjc.com/news/covidace2.
General Website Link. - March 17, 2020. “Report Sulle Caratteristiche Dei Pazienti Deceduti Positivi a COVID-19 in Italia Il Presente Report è Basato Sui Dati Aggiornati al 17 Marzo 2020.”

https://www.epicentro.iss.it/coronavirus/bollettino/Report-COVID-2019_17_marzo-v2.pdf.
PDF. - March 18, 2020. Tommaso Ebhardt, Chiara Remondini, and Marco Bertacche. “99% of Those Who Died From Virus Had Other Illness, Italy Says.” Bloomberg.

https://www.bloomberg.com/news/articles/2020-03-18/99-of-those-who-died-from-virus-had-other-illness-italy-says.
Magazine. - November 7, 2020. Marco Festa, Clementina Sansone, Christophe Brunet, Fabio Crocetta, Luisa Di Paola, Michele Lombardo, Antonino Bruno, Douglas M. Noonan, and Adriana Albini. “Cardiovascular Active Peptides of Marine Origin with ACE Inhibitory Activities: Potential Role as Anti-Hypertensive Drugs and in Prevention of SARS-CoV-2 Infection.” International Journal of Molecular Sciences 21 (21): 8364.

https://doi.org/10.3390/ijms21218364.
Research Journal.
Medications Used For High Blood Pressure
ACE inhibitors (ACEi) are derived from a factor in the venom of the Bothrops jararaca, a South American pit viper.
If Dr. Bryan Ardis’s theory about snake venom is correct, then it is possible that a combining of snake venom products is what is increasing risks.
Angiotensin receptor blockers (ARB) appear to be the result of chemical experimentation.
Given the increased risks for those taking ACE inhibitors or angiotensin receptor blockers, the question became whether medications should be changed or stopped during COVID-19. The purpose of the NephJC article is to explore this question.
Sources:
- “ACE Inhibitor.” In Wikipedia.

https://en.wikipedia.org/w/index.php?title=ACE_inhibitor.
Reference. - “Angiotensin II Receptor Blocker.” In Wikipedia.

https://en.wikipedia.org/w/index.php?title=Angiotensin_II_receptor_blocker.
Reference. - “Discovery and Development of Angiotensin Receptor Blockers.” In Wikipedia.

https://en.wikipedia.org/w/index.php?title=Discovery_and_development_of_angiotensin_receptor_blockers.
Reference.
See also, on this site:
Brief Overview of Blood Pressure Biochemistry
The regulatory system for blood pressure is explained as follows:
The renin–angiotensin–aldosterone system (RAAS) regulates the blood pressure. Renin, produced by kidneys to counteract decrease blood flow, cleaves its substrate hormone angiotensinogen, generating the decapeptide Angiotensin I that is in turn cleaved by Angiotensin-converting enzyme (ACE) to produce the angiotensin II (Ang II). Ang II binds to its receptor on the cell surface AT1R inducing vasoconstriction, renal sodium (Na+) reabsorption, and Aldosterone secretion, thereby increasing blood pressure and bringing a higher flux to the kidneys. The angiotensin-converting enzyme 2 (ACE2) cleaves Ang II to Ang (1–7), binding to MES, and causes vasodilation and cardioprotection. ACE2 is a “protective” enzyme to downregulate high blood pressure and inflammation.
Sources:
- November 7, 2020. Marco Festa, Clementina Sansone, Christophe Brunet, Fabio Crocetta, Luisa Di Paola, Michele Lombardo, Antonino Bruno, Douglas M. Noonan, and Adriana Albini. “Cardiovascular Active Peptides of Marine Origin with ACE Inhibitory Activities: Potential Role as Anti-Hypertensive Drugs and in Prevention of SARS-CoV-2 Infection.” International Journal of Molecular Sciences 21 (21): 8364.

https://doi.org/10.3390/ijms21218364.
Research Journal. - “The Renin-Angiotensin-Aldosterone System (RAAS).” Straight Healthcare.

https://www.straighthealthcare.com/renin-angiotensin-aldosterone-system-figure.html.
General Website Link.
Potential Remedies
In this setting, recombinant ACE2, angiotensin1-7 and angiotensin II type 1 receptor blockers could be promising therapeutic approaches in patients with SARS-CoV-2 infection.
Newly published research (June 2021) shows Dandelion can stop the engineered spike protein from binding to the ACE2 receptors (main entry point for SARS-Cov2) on cell membranes.
A German university study found that the common dandelion (Taraxacum officinale) can block spike proteins from binding to the ACE2 cell surface receptors in human lung and kidney cells. The water-based dandelion extract, taken from the plant’s dried leaves, was effective against spike protein D614 and a host of mutant strains, including D614G, N501Y, K417N and E484K.
SARS-CoV-2 is steadily mutating during continuous transmission among humans. This might eventually lead the virus into evading existing therapeutic and prophylactic approaches aimed at the viral spike. We found effective inhibition of protein-protein interaction between the human virus cell entry receptor ACE2 and SARS-CoV-2 spike, including five relevant mutations, by water-based common dandelion (Taraxacum officinale) extracts. This was shown in vitro using human kidney (HEK293) and lung (A549) cells, overexpressing the ACE2 and ACE2/TMPRSS2 protein, respectively. Infection of the lung cells using SARS-CoV-2 pseudotyped lentivirus was efficiently prevented by the extract. The results deserve more in-depth analysis of dandelions’ effectiveness in SARS-CoV-2 prevention and now require confirmatory clinical evidence.
⋮
Our research was conducted using water-based extracts from plant leaves. We found that leaf extracts efficiently blocked spike protein or its mutant forms to the ACE2 receptor, used in either pre-or post-incubation, and that high molecular weight compounds account for this effect.
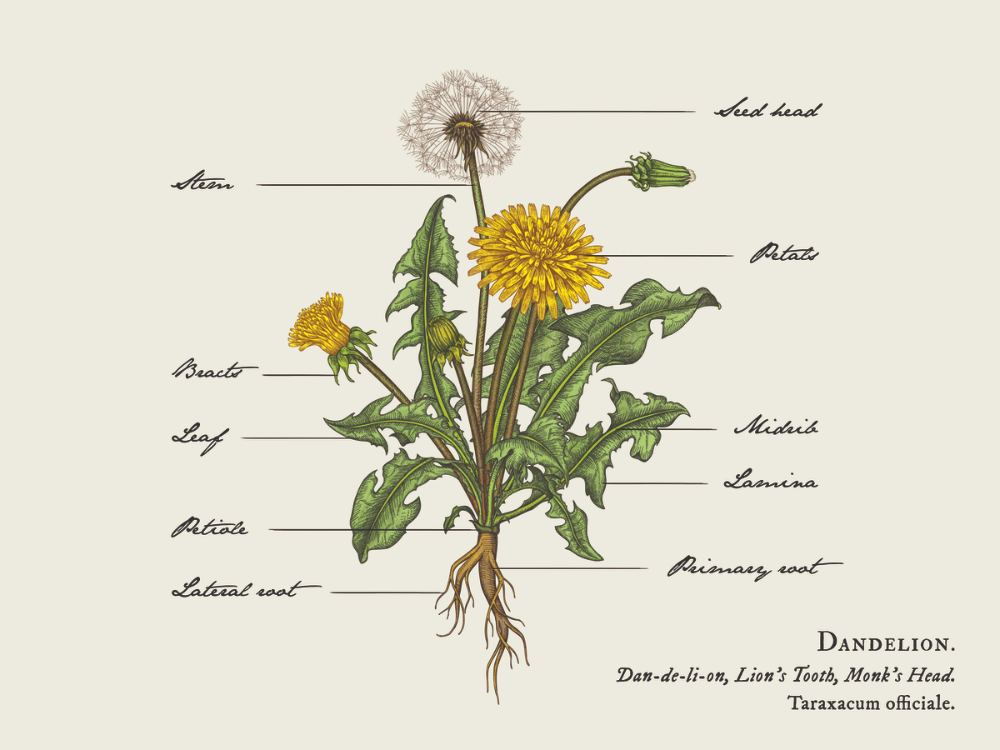
Dandelion Illustration by Yokaona
It does not appear that either of these potential treatments have been studied in humans for this exact syndrome. If you choose to purchase a dandelion leaf extract, please read the labels carefully. Dandelion extracts are made from any of or any combination of the roots, leaves, or flowers of the dandelion plant. Make sure that the extract you choose includes at least the leaves, since the water-based extract of that part of the plant is what was studied.
Please consult a physician, especially if you are taking any medications. There is a potential for interactions. Adjustments may need to be made to your other medications.
Sources:
- April 20, 2020. Paolo Verdecchia, Claudio Cavallini, Antonio Spanevello, and Fabio Angeli. “The Pivotal Link between ACE2 Deficiency and SARS-CoV-2 Infection.” European Journal of Internal Medicine 76 (April): 14–20.

https://doi.org/10.1016/j.ejim.2020.04.037.
Research Journal. - March 19, 2021. Hoai Thi Thu Tran, Nguyen Phan Khoi Le, Michael Gigl, Corinna Dawid, and Evelyn Lamy. “Common Dandelion (Taraxacum Officinale) Efficiently Blocks the Interaction between ACE2 Cell Surface Receptor and SARS-CoV-2 Spike Protein D614, Mutants D614G, N501Y, K417N and E484K in Vitro.” bioRxiv.

https://doi.org/10.1101/2021.03.19.435959.
Research Journal. - March 23, 2021. Liji Thomas. “Dandelion Extract Inhibits SARS-CoV-2 in Vitro.” News-Medical.Net.

https://www.news-medical.net/news/20210323/Dandelion-extract-inhibits-SARS-CoV-2-in-vitro.aspx.
News. - November 29, 2021. “Dandelion Leaf Extract Blocks Spike Proteins From Binding To ACE2 Receptors On Cells.” Holistic Health Online.

https://www.holistichealthonline.info/dandelion-leaf-extract-blocks-spike-proteins-from-binding-to-ace2-receptors-on-cells/.
Blog.
This article originated from a source that is behind a pay wall and therefore does not serve as a good reference. If you are interested in the original source, please see the citation at the bottom of the article. - Yokaona. “Dandelion Illustration.” Dribbble.

https://dribbble.com/shots/5955986-Dandelion-Illustration.
General Website Link.
Related:
- August 13, 2020. Yousef Tizabi, Bruk Getachew, Robert L. Copeland, and Michael Aschner. “Nicotine and the Nicotinic Cholinergic System in COVID-19.” The FEBS Journal 287 (17): 3656–63.

https://doi.org/10.1111/febs.15521.
Research Journal. - September 14, 2020. A. Sofia F. Oliveira, Amaurys Avila Ibarra, Isabel Bermudez, Lorenzo Casalino, Zied Gaieb, Deborah K. Shoemark, Timothy Gallagher, Richard B. Sessions, Rommie E. Amaro, and Adrian J. Mulholland. “Simulations Support the Interaction of the SARS-CoV-2 Spike Protein with Nicotinic Acetylcholine Receptors.” BioRxiv: The Preprint Server for Biology, September, 2020.07.16.206680.

https://doi.org/10.1101/2020.07.16.206680.
Research Journal. - “Nicotinic Acetylcholine Receptor.” In Wikipedia.

https://en.wikipedia.org/w/index.php?title=Nicotinic_acetylcholine_receptor.
Reference. - “Receptor Antagonist.” In Wikipedia.

https://en.wikipedia.org/w/index.php?title=Receptor_antagonist.
Reference.